I recently had surgery and interestingly, during my last placement I cared for people who had the exact same surgery that I’ve just had. So naturally, I went to my pre-op thinking that I knew everything that I would need to know. On the day of my surgery, I knew in my head the exact order in which things would need to happen…admission, WHO safety checklist, consent, TED stockings, no jewellery etc.. multiplied by 3. Then sleep. Then wake up. Then recovery. Home.
It wasn’t that simple. I was in pain – did I want to press the call bell? No, I didn’t want the nurses to think I was making it up and that I was a trouble maker. I couldn’t get comfortable. I wanted another pillow. I wanted an orangey drink because I hadn’t drank or eaten for hours and water was just not going down too well with me. I was hungry but didn’t want soup because my hands were shaking and I was worried that I would spill it all over myself. I ate it anyway. I needed the toilet but didn’t want to cause a fuss and have to unplug oxygen, BP cuff, cardiac monitor, pulse oximeter etc.. off me to then have to plug it all back on so I held it in until I could no longer hold it in any more. My lips were dry and I wanted lip balm which I didn’t have so I just licked and licked them until they got sore. I was cold and wanted to put my own pyjamas on. My hair was a mess and I wanted it in a bun on the top of my head and out of the way but with all the various things I had plugged onto me I couldn’t get to my hair so I just sat there looking like a hairy monster. Not that it mattered much because I also couldn’t see anything – my glasses were in my bag.
When I eventually got home (after a longer than expected stay in hospital due to a reaction to anti-sickness meds) I had no idea what to do with my medication, or when I would have my follow up, or how long to rest for. I had no clue. I had been told all of this before my discharge but retained none of it.
I thought I knew what to expect. But I really didn’t. I thought that I knew what patients that I had previously cared for had gone through. Not really!
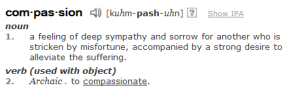
Here is the definition of compassion:
Honestly, I’m worried now. Would I have known what it was like to have this surgery when I was on placement I think I would have been much more attentive to patients. Not that I neglected them but now I’m not so sure that I was able to really empathise at the time. I’m not sure that I would have been able to alleviate their suffering just like the definition says without knowing what it was! I can’t possibly have every procedure and intervention known to man in order to know what it feels like for patients, so how can I be completely compassionate without really understanding?
These are rhetorical questions of course. I’m not sure I will ever be able to fully understand. But I can try. I believe that now I know what kind of questions to ask post-surgical patients and this is where communication is key. Maybe I can even apply them to all patients. I think it’s definitely work in progress but I’m grateful for the very personal experience and I hope that it will make me a much better and compassionate nurse in the long term.