Peru is very different to what we are accustomed to here in the UK. For starters, they don’t have the NHS. So, my elective placement was definitely guaranteed to be a million miles away from anything I could have encountered throughout my nursing programme at home. I was based in a private clinic called Clinca Peruano Suiza – a 14 (ish) bed elective and emergency treatment centre (You will see why the bed count is a little iffy further on!)
Being on a nursing degree programme, my elective placement very much focused on nurses and their practice so you will have to forgive me if I make little reference to other health professionals – who were clearly very much present! The nurses in Clinica Suiza differed from the nurses I have encountered so far for a number of reasons.
- Firstly, they worked in a private clinic. In Peru, most people require private health insurance to access health services as public services, unlike in the UK, are scarce.
- There is also a high patient to nurse ratio. Whilst the number of patients seen in total at the clinic is much lower than the average UK hospital there is only one nurse caring for all inpatients (which is usually around 14). There are also less nurses available for every doctor. In the UK, the average is 3 nurses for every 1 doctor whilst in Peru is one nurse for every doctor. In practice, this means that there are less nurses available for doctors to delegate work to.
- Being a private clinic, nurses encountered a number of ‘predictable’ patient groups. Because of the need for medical insurance, or sufficient finances to pay for treatment, the type of patients seen at the clinic generally fell into the following categories:
- Firstly, Emergencies – so this covered anyone who did not really have time to decide how they are paying for treatment.
- Tourists – who were generally armed with several travel and medical policies and could therefore afford most treatments.
- And the third, the “wealthier” Peruvian who could afford insurance. Although it is all relative and they were still comparatively poor – actually around 58% of the population could not afford any medical cover whatsoever. It’s nice to have free healthcare eh?
- Interestingly, in the time that I observed these nurses, there were no patients seen with minor injuries. It certainly made an impression on me having spent a placement in A&E in the UK and having observed some of the complaints the people present with! I think Peruvians are savvier and self-care much more. There are pharmacies on every street corner probably proves this point.
- Nurses at the clinic also managed and trained a team of nursing technicians. The role of a nurse technician was somewhere between a care support worker and an assistant practitioner which I’m not sure exists in the UK. At the clinic there was one nurse for every 3 technicians.
- They also wrote their own drugs kardexes or prescriptions – under the supervision of the doctor but it was often the nurse guiding the pharmacist on the medication required. I think, this was again associated to the cost of treatment, as even syringes were ordered on prescription and charged for!
- Finally, these nurses whilst they were non-specialised they were very highly skilled in general nursing, paediatrics and midwifery as the low number of nurses available required that they were all able to undertake any sort of emergency! So there was no need for them to study the branches that we are accustomed to here in the UK. Nurse education is also 5 years long instead of 3 such as in UK.
Of course, there are similarities and many universal roles that nurses have to take on in Peru that reflect the roles of the nurses I have encountered in placement in the UK. Assisting with ADLs, documentation, drug administration, advocacy, coordinating care and communication I think are all part of the global role of the nurse.
Communication was a funny one – I speak Spanish fluently and expected that once in Peru I would be able to fully understand everything but I quickly realised that speaking the same words does not mean that you speak the same language. It is a much more complex relationship. The nurses that I observed did not often talk to patients directly, talking to the patient was seen as the traditional role of the doctor, who often spoke multiple languages. But nurses still acted as advocates for their patients and often offered clear and effective insight and feedback to the doctor in front of the patient. On one hand this could be a good process as it provides one single source of verbal information. On the other hand, this could make the patient feel that he or she is being talked about rather than talked to.
In terms of written communication, nurses in Peru used colour coding to note information – in blue pen for morning shifts, and red for evening shifts. The colour makes information stand out and seemingly more interesting to read! The colour coding also continued in the drugs and nursing kardexes with procedures in blue ink and medications in red. Black pens were banned! I asked a number of times why blue and red were used and I’m not sure I ever got a straight answer – although perhaps I just didn’t understand it!
The nurses that I observed would also often keep their distance and provide little therapeutic touch unless a procedure was required. Whilst this sounds standoffish, this detachment I think is very much a Peruvian trait – within their culture remaining at a distance is a sign of respect – a fact that was often misrepresented by nurses and mutually misunderstood by tourists!
Similarly, the tone and character of voice used by Peruvian nurses was also a little surprising at times. Peruvians use the diminutive form in much of their vocabulary. Imagine adding ‘little’ or ‘wee’ to every word in a sentence then multiply it by 10 and you are probably close to Peruvian Spanish. Whilst it can come across as a form of endearment and familiarity it can sometimes feels like this diminishes the urgency of illness and treatment. For example, a patient who had recently arrived in Cusco (which sits at an altitude of over 3200 metres above sea level) was advised that he was ‘lacking a little bit of oxygen’. Saturations were 52% and the patient was clearly suffering from dangerous altitude sickness! I’m not sure that was the most appropriate way to describe the patient’s condition!
Appearance was also an interesting concept! The nurses I observed wore scrubs of different colours to represent their status and were immaculately turned out. One thing I noted was that nurses in Cusco o ften wore long sleeves, coats and scarves during their day to day nursing practice. There was just no other way to manage….it was so cold even in the hospital as there is no heating anywhere in the city! It could be argued that this is an infection risk but I wonder if bacteria could even grown in those temperatures 😉 and who would convey a more effective and positive message? A warm nurse wearing appropriate clothing for the temperature or a shivering nurse with a snotty nose baring her elbows? Nurses needs to evolve their means of communication, whatever they may be, in order to communicate in a manner that is adequate and relevant to their surroundings. I worked a number of night shifts and wore several layers under my scrubs to ensure I was somewhat warm. It was not pleasant!
ften wore long sleeves, coats and scarves during their day to day nursing practice. There was just no other way to manage….it was so cold even in the hospital as there is no heating anywhere in the city! It could be argued that this is an infection risk but I wonder if bacteria could even grown in those temperatures 😉 and who would convey a more effective and positive message? A warm nurse wearing appropriate clothing for the temperature or a shivering nurse with a snotty nose baring her elbows? Nurses needs to evolve their means of communication, whatever they may be, in order to communicate in a manner that is adequate and relevant to their surroundings. I worked a number of night shifts and wore several layers under my scrubs to ensure I was somewhat warm. It was not pleasant!
But that wasn’t the worst thing. I felt frustrated by the fact that patients were restricted on the care they could receive by the cover of their insurance policies or their finances, and often could not afford the treatment they would rather have, but instead, had to have the treatment their insurance dictated. Often going without vital medication. However, the doctors were very open and only suggested treatments or investigation they
 felt were necessary. Nurses in Peru faced very conflicting and difficult situations as they were often bound by a strict medical model rather than the holistic nursing model we aim for in the UK. Nonetheless, in my experience they were able to provide effective and prompt care to the best of their ability. Indeed, the care a patient experienced was also very much affected by resources available as well as technology. Resources were tight. Nothing is Cusco was new nor shiny – much equipment was re-used multiple times, for example saline bottles were also used as ‘sharps boxes’. Actually, I found this very refreshing and resourceful – I never had once had that ‘what a waste!’ moment.
felt were necessary. Nurses in Peru faced very conflicting and difficult situations as they were often bound by a strict medical model rather than the holistic nursing model we aim for in the UK. Nonetheless, in my experience they were able to provide effective and prompt care to the best of their ability. Indeed, the care a patient experienced was also very much affected by resources available as well as technology. Resources were tight. Nothing is Cusco was new nor shiny – much equipment was re-used multiple times, for example saline bottles were also used as ‘sharps boxes’. Actually, I found this very refreshing and resourceful – I never had once had that ‘what a waste!’ moment.
Going back to those beds….family involvement in Peru is expected, and in fact, an extra bed was always made available for family in the same room as the patient at the clinic. So whilst there were 14 inpatient beds, there were actually 28 once we counted the extra ones for relatives. I would imagine that if the hospital got very busy that those beds would then be used for patient care. But, the point to take is that the involvement of relatives and significant ones meant that not only did they take some of the responsibility of caring for their loved one but it also meant that the patient had support as and when needed rather than having to wait until visiting hours! This facilitated great individualised and inclusive care for patients, something that we strive for so much in the UK.
What I liked the most about the MDT in Clinica Peruano Suiza was that every member of the MDT was present during ward rounds. This included pharmacists in charge of dispensing medication, the admin staff in charge of updating the insurance companies, the surgeon if relevant, doctors, nurses and all technicians. This meant that all members of the MDT were updated and handover over to at the same time. Although I appreciate that this is possible in a small clinic and may not be feasible in a larger hospital, I felt that this enhanced the handover process and prevented information being missed ultimately ensuring that the best, most efficient and prompt care and treatment for the patient.
I mentioned earlier that nursing education in Peru is longer than in the UK. However, nurses not required to be registered so it could be argued that without a regulating body the quality of nursing care given to a patient could be affected – there are however minimum educational global standards to be met and from what I observed, the whole MDT worked together to ensure the right mix of knowledge and skills were available to provide effective and individual patient care at all times – calling upon in-house specialists and surgeons as needed to improve the quality of service through an inter-professional approach. But this can vary greatl y between public and private health services. Public hospitals in Peru have been on strike since 13th May 2014 and are only open to emergencies with most patients having to pay for private healthcare. This is a political move in support of improved terms and conditions for workers. It is greatly benefitting private clinics such as Clinica Peruano Suiza but at the great detriment and expense of the neediest patients whose needs are not being met by the very organisations and agencies set up to care for them. Could you imagine the NHS closing down for even one day? Me neither!
y between public and private health services. Public hospitals in Peru have been on strike since 13th May 2014 and are only open to emergencies with most patients having to pay for private healthcare. This is a political move in support of improved terms and conditions for workers. It is greatly benefitting private clinics such as Clinica Peruano Suiza but at the great detriment and expense of the neediest patients whose needs are not being met by the very organisations and agencies set up to care for them. Could you imagine the NHS closing down for even one day? Me neither!
The lack of sanitation facilities and adequate water supplies in Cusco posed different priorities of care for nurses and the MDT, with communicable diseases and food and waterborne illnesses being much more common among the indigen ous populations than the colonial societal groups – who were more likely to suffer from lifestyle and excess conditions such as diabetes, obesity and alcoholism. Similarly, nurses often had to consider tradition and religion in their patient care although this often caused conflicts of interest. For example, the use of coca tea is widely recommended in Peru by traditional healers for altitude sickness and patients were often reluctant to take medications as prescribed in favour of traditional cures! I heard many a conversation where doctors and nurses were unsuccesful in trying to educate patients on the use of medications in conjunction with more traditional remedies.
ous populations than the colonial societal groups – who were more likely to suffer from lifestyle and excess conditions such as diabetes, obesity and alcoholism. Similarly, nurses often had to consider tradition and religion in their patient care although this often caused conflicts of interest. For example, the use of coca tea is widely recommended in Peru by traditional healers for altitude sickness and patients were often reluctant to take medications as prescribed in favour of traditional cures! I heard many a conversation where doctors and nurses were unsuccesful in trying to educate patients on the use of medications in conjunction with more traditional remedies.
So…that was my placement area and the environment in which I spent my elective placement! Coming up soon…what did I learn?
 ften wore long sleeves, coats and scarves during their day to day nursing practice. There was just no other way to manage….it was so cold even in the hospital as there is no heating anywhere in the city! It could be argued that this is an infection risk but I wonder if bacteria could even grown in those temperatures 😉 and who would convey a more effective and positive message? A warm nurse wearing appropriate clothing for the temperature or a shivering nurse with a snotty nose baring her elbows? Nurses needs to evolve their means of communication, whatever they may be, in order to communicate in a manner that is adequate and relevant to their surroundings. I worked a number of night shifts and wore several layers under my scrubs to ensure I was somewhat warm. It was not pleasant!
ften wore long sleeves, coats and scarves during their day to day nursing practice. There was just no other way to manage….it was so cold even in the hospital as there is no heating anywhere in the city! It could be argued that this is an infection risk but I wonder if bacteria could even grown in those temperatures 😉 and who would convey a more effective and positive message? A warm nurse wearing appropriate clothing for the temperature or a shivering nurse with a snotty nose baring her elbows? Nurses needs to evolve their means of communication, whatever they may be, in order to communicate in a manner that is adequate and relevant to their surroundings. I worked a number of night shifts and wore several layers under my scrubs to ensure I was somewhat warm. It was not pleasant! felt were necessary. Nurses in Peru faced very conflicting and difficult situations as they were often bound by a strict medical model rather than the holistic nursing model we aim for in the UK. Nonetheless, in my experience they were able to provide effective and prompt care to the best of their ability. Indeed, the care a patient experienced was also very much affected by resources available as well as technology. Resources were tight. Nothing is Cusco was new nor shiny – much equipment was re-used multiple times, for example saline bottles were also used as ‘sharps boxes’. Actually, I found this very refreshing and resourceful – I never had once had that ‘what a waste!’ moment.
felt were necessary. Nurses in Peru faced very conflicting and difficult situations as they were often bound by a strict medical model rather than the holistic nursing model we aim for in the UK. Nonetheless, in my experience they were able to provide effective and prompt care to the best of their ability. Indeed, the care a patient experienced was also very much affected by resources available as well as technology. Resources were tight. Nothing is Cusco was new nor shiny – much equipment was re-used multiple times, for example saline bottles were also used as ‘sharps boxes’. Actually, I found this very refreshing and resourceful – I never had once had that ‘what a waste!’ moment. y between public and private health services. Public hospitals in Peru have been on strike since 13th May 2014 and are only open to emergencies with most patients having to pay for private healthcare. This is a political move in support of improved terms and conditions for workers. It is greatly benefitting private clinics such as Clinica Peruano Suiza but at the great detriment and expense of the neediest patients whose needs are not being met by the very organisations and agencies set up to care for them. Could you imagine the NHS closing down for even one day? Me neither!
y between public and private health services. Public hospitals in Peru have been on strike since 13th May 2014 and are only open to emergencies with most patients having to pay for private healthcare. This is a political move in support of improved terms and conditions for workers. It is greatly benefitting private clinics such as Clinica Peruano Suiza but at the great detriment and expense of the neediest patients whose needs are not being met by the very organisations and agencies set up to care for them. Could you imagine the NHS closing down for even one day? Me neither!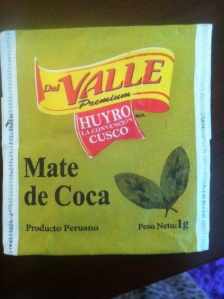 ous populations than the colonial societal groups – who were more likely to suffer from lifestyle and excess conditions such as diabetes, obesity and alcoholism. Similarly, nurses often had to consider tradition and religion in their patient care although this often caused conflicts of interest. For example, the use of coca tea is widely recommended in Peru by traditional healers for altitude sickness and patients were often reluctant to take medications as prescribed in favour of traditional cures! I heard many a conversation where doctors and nurses were unsuccesful in trying to educate patients on the use of medications in conjunction with more traditional remedies.
ous populations than the colonial societal groups – who were more likely to suffer from lifestyle and excess conditions such as diabetes, obesity and alcoholism. Similarly, nurses often had to consider tradition and religion in their patient care although this often caused conflicts of interest. For example, the use of coca tea is widely recommended in Peru by traditional healers for altitude sickness and patients were often reluctant to take medications as prescribed in favour of traditional cures! I heard many a conversation where doctors and nurses were unsuccesful in trying to educate patients on the use of medications in conjunction with more traditional remedies.