As I mentioned in my previous entry. I want to write about each of the 6Cs (have a look at my ‘6 C’ing my way through nursing’ entry if you want to know more!)
I wanted my first entry to be about Courage – for no other reason than a couple of events this week have really made me reflect on why people do certain things, and in turn, why I do the things that I do. Worth pointing out that in my view (and you may disagree here) there is a very distinct difference between being courageous and being reckless – though I accept that different people see things very differently. Nonetheless, I like to think I am the former and not the latter. So here goes….
When I resigned from my previous job, people said I was making a rash decision; a whim they called it. Those who knew me little were surprised at my new career choice. Those who know me best reacted with “about time” comments and those people were simply full of admiration. How many people do you know who are stuck in a rut? It may be work, it may be the house they live in, it may be a relationship, it may be financial worries or all of the above! It may even be you – reading this now – who is feeling like that..and how many people have the courage to make change happen? How many of all those people have the courage to change their circumstances? As it stands, I have met a lot of nurses and student nurses who have found that courage. Every single one of the people I have cared for are courageous people. They have courage to carry on; to keep trying; to keep smiling.
Take Dr Kate Granger, she’s a GP diagnosed with a very rare and terminal cancer. I have been very lucky to have met her, and can honestly say I have never met anyone so honest, open and courageous…unafraid to fight for what she believes in. She has fought tooth and nail for our NHS and to raise awareness of the value of person centred care and she has continued to do in the little time she has left. She has talked openly about her experiences in hospital as a patient and offered much valuable feedback on how we can improve further. Not as a means to devalue the NHS but in order to make it even better than it already is. This includes her ‘Hello, my name is’ campaign – encouraging all health workers to introduce themselves to patients as a matter of course. She’s a boat rocker and one of the very bravest.
Then, take the Daily Mail <sigh>….. I really wish I could remain objective when writing about such a sensationalist paper. This week, it published a story about Dr Granger’s campaigning. They didn’t really listen, they didn’t understand and without any consideration to Dr Granger turned HER story into one of disappointment and despair – Kate Granger is nothing like that. She is positive, encouraging and ambitious and the Daily Mail have broken her heart…but she has picked it back up, and has vowed to continue all her hard graft. What an inspirational lady.
What do you think? Who is courageous or who is reckless? Does it depend?
The thing with courage is that people think that a heroic act is needed in order to be courageous. I’m not sure I believe that. I take courage as I take risk. I weigh up cost vs benefit. Most of all do this in our daily lives anyway. To have a salad or a pizza. To drive or take the bus. To hang the washing out when its cloudy or not. To drive those extra 5 miles with the petrol warning light on or not. They are all decision that we make daily and risks that we take each and every day. They are all rational and calculated risks for which we accept the consequences. In my eyes, courage encompasses the ability to accept responsibility for the consequences of our actions – possibly to the benefit of others and not ourselves – and to do it regardless, much like Dr Granger does each and every day.
How would you define courage? Dictionaries not allowed.
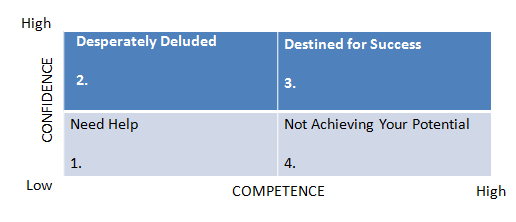
Sometimes I wonder how people like Dr Granger do it. Where do they find the strength? I aim for the same bravery or course. Whether I will get there it remains to be seen! I don’t often say no to a new opportunity or to a challenge. If you have never seen the ‘Yes Man’ with Jim Carrey I would certainly encourage you to. I may have mentioned this in previous blogs but its a great film and incredibly inspiring. It is only because of this ethos that I have taken advantage of opportunities as much as I have. I don’t wait for other people to try things out first. I don’t wait for encouragement or coaxing. I like breaking down barriers and I’m not afraid of a little hard work to make it happen. I have to admit that recent experiences would suggest that hard work and success offend people, and they get really angry. I’m not very sure why but it makes no difference to me whatsoever. I truly believe that THERE ARE people out there with no agenda. I work hard because it’s the way I am made and to ask me to do something less than my best would go against everything that I believe in.
Because of this, I spend a lot of time reflecting on things that I have done and said and I try to rationalise all outcomes. I get happy, I upset, I pick myself up and I carry on. I do that almost constantly because I am so self aware that I analyse almost every single one of my moves. I am my biggest critic, as most people are. But I try to not give myself a hard time if I am wrong even if it takes a lot of effort and energy to let things go. This is incredibly difficult to put into practice – but I do try!
I understand that when I write this blog and publish it to the Universe that I make myself vulnerable by opening up myself and my thoughts and inviting feedback. I understand that the power of the internet means that whilst I open up to all my readers, that in turn my readers are able to hide behind an internet persona without consequence. The internet, or the freedom of press and speech (see the Daily Mail for example) gives people courage to perhaps do and say things that they would not otherwise do or say in ‘real life’. I know it certainly gives me courage to write things I would normally reserve for my ‘Dear Diary’ moments. In spite of that, I continue to do what I do, I continue to publish blog entries.
I don’t really want to apologise for the long entry. I feel that it is important that we are all self aware of our actions and whether you are in a caring profession or not, consider the 6Cs in every day life. In the context of this post perhaps you could consider, are you courageous or reckless? Does it depend? And if so, what on?
“Courage is what it takes to stand up and speak; courage is also what it takes to sit down and listen.” Winston Churchill
“Courage is grace under pressure” Ernest Hemingway